75 year old female patient with hypovolemic shock /(?) cardiogenic shock with type 1 respiratory failure and severe metabolic acidosis .
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her guardian’s signed informed consent.
Here we discuss our individual patient's problems through a series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective, current, best evidence based inputs.
This e-log book also reflects my patient centered online learning portfolio and your valuable inputs in the comment box is welcome.
NAME :: M.VARUN SAI
ROLL.NO. :: 73
BATCH :: 2017
A 75 year old female patient was brought to the casualty with chief complaints of
# FEVER since 4 days .
# GENERALISED WEAKNESS since 3 days .
# VOMITING since 3 days .
# SHORTNESS OF BREATH since 1 day.
History of presenting illness :
Patient was apparently asymptomatic 3 months back and is able to do her regular work at home.
she developed shortness of breath of grade 3 along with dizziness and generalised weakness which made her to fall for which she was taken to a local hospital in hyderbad , MRI was done which showed no abnormality and used medications for the above. There were no similar episodes when on medications.
4 days back she developed fever which was low grade , intermittent, not associated with chills and rigor , no diurnal variation , relieved on medications.
2 days back she developed vomitings of 4 episodes which were non projectile , food particles as content , non bilious , non foul smelling and associated with loss of appetite ( patient's attender gives the history that she often forgets to eat food )not associated with loose stools and pain abdomen.
She developed shortness of breath since morning which was grade 3 not associated with chest pain , palpitations, orthopnea and paroxysmal nocturnal dyspnea .
Past history ::
No similar compliants in the past and no previous hospitalization.
Not a known case of diabetes , hypertension, asthma , Tuberculosis and epilepsy.
No past surgeries and blood transfusion.
Personal history ::
Appetite is decreased.
Mixed diet.
Sleep adequate .
Bowel and bladder regular .
No known food and drug allergies.
No addictions.
Family history ::
Not significant.
GENERAL EXAMINATION ::
* The patient is conscious , non coherent and non -cooperative .
* Moderately built and moderately nourished.
Examined the patient in supine position and in well lit room.
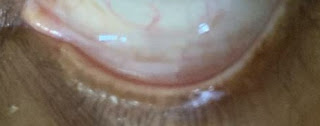
* Pallor : Absent
* Icterus : Absent
* Cyanosis : Absent
* Clubbing : Absent
* Lymphadenopathy : Absent
* Edema : Bilateral, pitting type upto thighs
VITALS ::
Temp: Afebrile
PR: 78 Beats per minute , low volume pulse , normal character and rythmn and vessel wall normal .
BP: could not be measured.
RR: 28 cycles per minute.
Spo2 - 50% at Room air. 85% at 15 litres of oxygen.
GRBS- 43 mg/dL.
SYSTEMIC EXAMINATION ::
* RESPIRATORY SYSTEM : Normal Vesicular Breath Sounds Audible, Position of trachea is central, Bilateral air entry present
* CVS : S1 and S2 Heard, no murmurs, no thrills
* CNS : Higher mental functions normal , Cranial nerves: intact, No meningeal signs, GCS- 15/15 , deep tendon reflexes are normal , sensory system intact.
* PER ABDOMEN : scaphoid shape, Abdomen not distended with no scars, sinuses, engorged veins , No tenderness, No palpable mass, normal hernial orifices , Bowel sounds heard.
DIFFERENTIAL DIAGNOSIS ::
? Hypovolemic shock/cardiogenic shock. ? Starvation ketoacidosis.
? Toxic ingestion.
PROBABLE PATHOGENESIS FOR THE DISEASE ::
INVESTIGATIONS ::
PROVISIONAL DIAGNOSIS ::
HYPOVOLEMIC SHOCK/ (?) CARDIOGENIC SHOCK with type I RESPIRATORY FAILURE and SEVERE METABOLIC ACIDOSIS.
TREATMENT ::
1. 30 Normal saline bolus i.v.
2. 10 Normal saline infusion at 100ml/hr.
3. Injection Nor adrenaline ( 20mg + 30ml Normal saline ) at 8ml/hr. Increase or decrease the dose as required to maintain mean arterial pressure more than 65mm of Hg .
4. Oxygen inhalation to maintain saturation.
5. Patient was intubated around 7.30 pm on 11/01/2022 .












Comments
Post a Comment