66 years MALE with stage 5 CKD with type 2 respiratory failure with dyselectrolytemia secondary to renal loss or rta
M VARUN SAI ( INTERN)
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT
CHIEF COMPLAINTS :
C/O SOB since 1 week
C/O generalised swelling since 1 week
HOPI :
66 year old male, who is a father of 3 children ( 2 sons + 1 daughter).He used to sell the clothes by going to every village and take care of his family.
In 2011, patient had sudden onset chest pain, where he was taken to cardiologist and Angiogram was done , where the doctors told 3 vessels were blocked and Bypass surgery (CABG)was done.After his surgery , he stopped selling the clothes by going to Village and started a small shop were he used to sell the plastic material ( buckets, mugs etc ).
After 2 years ( in 2013), patient had Generalized weakness, where he was taken to hospital and found to be diabetic and hypertensive and started on medication.
Meanwhile patient had knee joint pains , where he used medication (pain killers ) from medical shop . According to daughter ,he almost used 10 years.
1 and 1/2 year back, patient developed pedal edema and shortness of breath on exertion, were he was taken to the hospital and found his renal parameters were deranged and started on conservative management.
Exactly 6 months back ( in July), the patient developed severe shortness of breath, and pedal edema worsened and patient was taken to nims , where central line was placed and started on hemodialysis ( 1 session done ).Then they came to our hospital and 3 sessions of hemodialysis done.Mean while , patient was in altered sensorium also, he pulled his central line, but not completely removed , after 3 sessions of hemodialysis,his sensorium improved.
Then he was taken to the hospital in Hyderabad, where he was suggested to have peritoneal dialysis and daily one session done.
The same peritoneal dialysis was done for 5 month.
On Feb 8th , patient was started on 3 sessions of peritoneal dialysis per day, but his shortness of breath was not controlled and so he was brought here for further evaluation.
PAST HISTORY :
K/C/O diabetes since 10 years and on regular medication.
K/C/O HTN since 10 years and on regular medication
K/C/O CAD 10 years ago and underwent CABG in 2011
Not a K/C/O asthma , epilepsy , tuberculosis , CVA , Thyroid disorders.
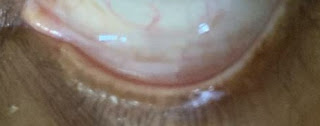
GENERAL EXAMINATION :
Pt is conscious , coherent , cooperative .
Moderately built and nourished.
No signs of pallor ,icterus, cyanosis , clubbing , lymphadenopathy , edema.
Vitals :
Temp. - 98.6F
PR - 96bpm
BP - 150/100 mmHg on admission
110/80 mmHg later
RR - 35cpm on admission
20cpm in ICU
Sats - 80% on RA , 94% on 14lts of O2.
SYSTEMIC EXAMINATION :
RS:
Inspection - symmetrical shape of chest,
Trachea central , a vertical scar of previous CABG present , no sinuses and engorged veins.
Palpation - no local rise of temperature , no tenderness , all inspectory findings are confirmed.
Trachea central. Trail sign absent .
Apex beat palpable at 5th intercostal space at midclavicular line.
Percussion -
Resonant note
Auscultation -
Diffuse Inspiratory crepitations are heard in all the areas.
Wheeze present .
CVS :
S1S2 heard , no added sounds.
CNS :
Higher mental functions are intact , no focal neurological deficits .
PER ABDOMEN :
obese abdomen , umbilicus central and inverted .
Soft , non tender .
No organomegaly.
Bowel sounds heard.
DIAGNOSIS :
CKD on MHD with dyselectrolytemia secondary to ?renal loss ?RTA.
INVESTIGATIONS:
TREATMENT :
Iv fluids @(urine output + 30ml/hr)
Inj. Lasix 40mg po/bd at 8am , 4pm
Inj. HAI s/c tid acc to GRBS.
Cpr was done 27/2/23 as his saturation levels fell and BP , pulse was not recordable.
Inj. Norad 2 ampule at 10ml/hr in 46ml NS ( increase or decrease according to MAP )
Inj. Dobutamine 1 ampule at 5ml/hr in 45ml NS ( increase or decrease according to MAP )
Inj. Fentanyl 2 ampule at 5ml/hr in 46ml NS
Inj. Atracurium 2 ampule at 5ml/hr in 46ml NS
Inj. Monocef 1gm iv/bd
Tab. Nodosis 500mg po/od
Tab.shelcal 500mg po/od.
Tab. Cinod 10mg po/bd
cap. BioD3 po/weekly twice












































Comments
Post a Comment