M VARUN SAI ( INTERN)
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis .
CHIEF COMPLAINTS :
C/O lower back ache since 2 years
C/O left sided chest pain since 1 year
HOPI :
pt was apparently asymptomatic 2 years back then she developed lower back pain since 2 years , insidious in onset , gradually progressive , radiating to lower limbs , aggravated on bending forward , relieved on taking rest .
C/O left sided chest pain intermittent in nature , dragging type , radiating to left shoulder , no aggravating and relieving factors , associated with shortness of breath on exertion.
No H/O orthopnea , PND , palpitations , burning micturition , constipation , loose stools, fever .
No H/O trauma .
PAST HISTORY :
No similar complaints in the past.
History of ? infection( according to patient) to the right eye at the age of 1 year and lost her vision in right eye since then.
Not a known case of DM2 , HTN , CVA , CAD , TB , ASTHMA , THYROID DISORDERS.
PERAONAL HISTORY :
Normal appetite
Sleep adequate
Bowel and bladder regular
Occasional toddy consumption.
GENERAL EXAMINATION :
Pt is conscious , coherent , cooperative
Moderately built and nourished
No pallor , icterus , clubbing , cyanosis , lymphadenopathy , edema.
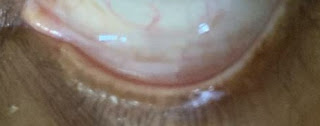
Right eye examination - A leucomatous opacity of the cornea with minimal vascularization present.
VITALS :
Temp- afebrile
PR-80bpm, normal rhythm , volume and character
RR-20cpm, thoracoabdminal
BP-110/70mmHg
Spo2-98% at room air
GRBS-101mg/dl
SYSTEMIC EXAMINATION :
CVS - S1,S2 Heard , no added murmurs
RS - Bilateral air entry present , normal vesicular breath sounds heard , no added sounds
CNS - HMF intact. , No focal neurological defect
PER ABDOMEN - obese abdomen , Soft , Non tender , no organomegaly , bowel sounds present .
DIAGNOSIS -
? LUMBAR SPONDYLOSIS.
CHEST PAIN UNDER EVALUATION.
INVESTIGATION :
DEGENERATIVE SPINE
LUMBAR SPONDYLOSIS
RIGHT EYE LEUCOMATOUS OPACITY
TREATMENT :
1. Tab.ultracet PO/BD
2. Tab.MVT PO/OD
3. Tab. Neurokind OD



















Comments
Post a Comment