55year old female with dengue and meningoencephalitis.
SHORT CASE - FINAL MBBS PART 2 PRACTICAL EXAMINATION.
Name : M VARUN SAI
REG. NO.: 1701006099
This is an online Elog book to discuss our patient deidentified health data shared after taking his/ her guardians sign informed consent.
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with n aim to solve those patient clinical problem with collect6current best evidence based input
This Elog also reflects my patient centered online learning portfolio.
Your valuable inputs on comment box is welcome
* I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whatsoever.
CASE REPORT ::
A 55year old female patient who is housewife hailing from nalgonda was brought to the hospital with
CHIEF COMPLIANTS ::
* Fever since 5 days .
* Neck stiffness since 5 days.
HISTORY OF PRESENT ILLNESS ::
Patient was apparently asymptomatic 5 days back and was able to perform her regular activities without any difficulty then she experienced
FEVER
sudden onset
Continuous
Associated with chills and rigor
Associated with generalised body pains and headache .
Associated with 1 episode of vomiting which is non projectile, non bilious , food particles as content and non foul smelling. Not associated with abdominal pain and loose stools.
Relieved on medication.
NECK STIFFNESS
Sudden onset
Associated with decreased range of movements at neck
No H/O trauma
Not relieved on rest and painkillers.
No H/O Burning micturition.
PAST HISTORY ::
No similar compliants in the past.
Not a known case of hypertension , Tuberculosis, epilepsy, asthma and CAD.
H/O CVA with compliants of bilateral upper & lower limb paralysis 7 years back for which she was treated and recovered in 1month .
Surgical H/O - Hysterectomy 25years back.
PERSONAL HISTORY ::
Diet - Mixed
Appetite - reduced
Sleep - adequate
bladder - regular
Bowel movements - constipation since 3 days
No addictions and no known allergies.
FAMILY HISTORY ::
Not significant.
GENERAL EXAMINATION ::
Patient is conscious, coherent, and cooperative.
Moderately built and nourished.
Well oriented to time, place and person.
Patient was examined in supine position in a well lighted room after taking consent and explaining the procedure.
PALLOR - absent
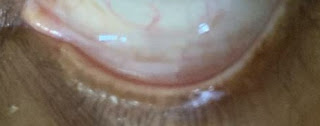
ICTERUS - absent
CLUBBING - absent
CYANOSIS - absent
LYMPHADENOPATHY - absent
EDEMA - absent
VITALS ::
Temperature - 99⁰F
Pulse rate - 98 beats per minute , normal volume , character and normal vessel wall , no radioradial and radiofemoral
delay .
Respiratory rate - 20cycles per minute
Blood pressure - 110/70 mmHg in both arms.
O2 sat. - 96% at room air.
SYSTEMIC EXAMINATION::
CNS EXAMINATION:
Higher mental functions : NORMAL
Cranial nerve examination :
All cranial nerves functions are intact.
Cerebellar examination : No abnormality detected
Sensory system examination - Normal .
Motor system -
Muscle bulk - normal in both upper and lower limbs.
Tone - normal in both upper and lower limbs.
Power - normal in both upper and lower limbs.
nuchal muscle stiffness present , slight tenderness over the neck.
Reflexes -
Biceps - present on both sides
Triceps - present on both sides
Supinator - present
Knee - present on both sides
Ankle - present on both sides
Plantar reflex - normal bilaterally.
Meningeal signs:
neck stifness - present
Kerning's sign - positive
Brudzinski's sign - positive .
Other system examination :
Cardiovascular system -
S1 , S2 heard , no murmurs.
Respiratory system examination -
Bilateral air entry present
Normal vesicular breath sounds
No advetitious sounds.
Per abdomen examination -
Soft and non tender
No organomegaly .
DIAGNOSIS:
? Viral infection with 2⁰ viral meningoencephalitis under evaluation.
INVESTIGATIONS ::
HEMOGRAM ::
MRI of BRAIN:
Findings : few areas of leptomeningeal enhancement in the sulcal areas of parietal and occipital region.
X RAY - SKULL& CERVICAL SPINE :
PROVISIONAL DIAGNOSIS :
Dengue fever with meningoencephalitis.
Denovo type 2 Diabetes mellitus.
TREATMENT ::
Inj. CEFTRIAXONE 2 gm/ BD
Inj.DEXAMETHASONE 6mg/iv/tid
Inj . Vancomycin 1gm/iv
Inj. Paracetomol 1gm/iv
Tab . Paracetomol 650 mg
Tab. Ecospirin 75 mg /po/od
Tab. Atorvastatin 10 mg /po/od
Syp. Cremaffin plus 30ml/po .













Comments
Post a Comment