60 yr female with pancreatitis and multiple gastroduodenal ulcers
M VARUN SAI ( INTERN)
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT
CHIEF COMPLAINTS :
c/o fever since 15 days
Abdominal pain since 15 days
Vomitings since 15days
HISTORY OF PRESENT ILLNESS :
Patient was apparently asymptomatic 3 months back then she had burning micturition, frothy urine, urgency, polyuria, nocturia,
No h/o polydypsia
Complaints of fever since 15 days, intermittent, low grade, associated with chills and rigors, releived by taking medication.
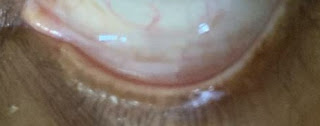
Epigastric pain since 15 days, squeezing type, tenderness present in epigastric region, no guarding, no rigidity, associated with vomitings, food as content, non projectile, non bilious, non foul smelling, 3-4 episodes of black coloured vomiting.
No loose stools, no chest pain, palpitations, Cough, cold
PAST HISTORY :
H/o split skin graft for right diabetic foot 4 years back
H/o left below knee amputation 1 year back
H/o hysterectomy
K/c/o TB 5 YEARS BACK
K/c/o DM since 20 years on mixtard insulin 20 units SC/od
K/c/o Hypertension since 1 year on T. Telma 40 and Amlo 5mg po/od
H/o blood transfusion of 8 units
PERSONAL HISTORY :
Housewife
Loss of appetite since 1 month
FAMILY HISTORY :
Her mother is a k/c/o DM
GENERAL EXAMINATION :
Patient is C/C/C
No signs of pallor, icterus, cyanosis, clubbing, generalised lymphadenopathy and pedal edema
A scar of previous split skin graft present ovet dorsum of right leg
Below knee amputated right leg.
Temp: afebrile
Pr: 86bpm
RR; 18cpm
Spo2: 98% @RA
GRBS: 398mg/dl
Systemic examination:
CVS: s1 s2 heard , no murmurs
RS: BAE present , NVBS , no added sounds
CNS : NFND , HMF intact
P/A : soft , non tender ,hysterectomy scar present , no organomegaly , bowel sounds present ,
DIAGNOSIS :
1. PANCREATITIS SECONDARY TO CHOLELITHIASIS
2. HYPERKALEMIA SECONDARY TO AKI
3. PSEUDOHYPONATREMIA
4. TYPE 2 DIABETES MELLITUS
5. HYPERTENSION
Rx:
1. NBM till further orders
2. IVF. NS @ 75ML/HR
3. INJ. PIPTAZ 2.25GM IV/TID
4. INJ. TRAMADOL 1 AMP IN 100ML NS IV
5. INJ. OPTINEURON 1 AMP IN 500ML NS IV/OD
6. INJ. PAN 40 MG IV/OD
7. INJ. ZOFER 4MG IV/SOS
8.INJ .MONOCEF 1GM IV/BD
9.H.PYLORI KIT PO/OD
10.SYP SUCRALFATE 10ml PO/TID before food
11. TAB. CINOD 10MG PO/OD



























Comments
Post a Comment