M VARUN SAI ( INTERN )
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis .
CHIEF COMPLAINTS :
C/O decreased appetite since 5months
C/O Abdominal distension since 5 days
C/O SOB since 5days
HOPI:
Pt. was apparently alright 5months back when she used to do her regular activities at home and go for work in the farms like picking weeds etc , then she had decreased appetite since 5months,then she developed Abdominal distension since 5 days,which was insidious in onset and gradually progressive in nature,she developed SOB which was insidious in onset and of grade 2.
There was no history of palpitations , orthopnea , PND , chest pain , cough . No history of fever , loose stools, vomitings , pain abdomen , constipation.
PAST HISTORY :
No similar complaints in the past .
N/K/C/O DM,HTN,TB, Epilepsy,CAD.
Hysterectomy was done 40yrs ago in view of ? heavy menstrual bleeding
Ovarian cystectomy ( cyst measuring 3.5kg) was done 12yrs ago i/v/o abdominal distension and abdominal pain.
Lap.cholecystectomy was done 8 yrs ago in view of symptomatic gall stones and choledocholithiasis.
ERCP and MRCP was done and diverticulum was found in the CBD.
She was diagnosed with ADPKD 12yrs back.
PERSONAL HISTORY :
Decreased appetite since 5months
Bowel habits decreased since 8 days
sleep adequate
Drinks Alcohol occasionally (stopped since 1 yr)
Had a habit of chewing ? Betel leaves along with sodalime for 1 year.
No known drug and food allergies .
GENERAL EXAMINATION :
Pt is conscious , coherent and cooperative .
Moderately built and has loss of buccal pad of fat .
NO signs of pallor , icterus , clubbing , cyanosis , lymphadenopathy and edema .
VITALS :
Temp- afebrile
PR-86bpm, normal rhythm , volume and character
RR-20cpm, thoracoabdminal
BP-110/80mmHg
Spo2-99% at room air
GRBS-101mg/dl
SYSTEMIC EXAMINATION :
CVS - S1,S2 Heard , no added murmurs
RS - Bilateral air entry present , normal vesicular breath sounds heard , no added sounds
CNS - HMF intact. , No focal neurological defect
Per abdomen :
Inspection :
Abdomen appears distended .
Umbilicus is central
An epigastric swelling of size 3x2cm with well defined margins, smooth surface , no impulse on coughing
A vertical scar is present in the suprapubic region.
No sinuses and engorged veins
Palpation :
No local rise of temperature .
No tenderness.
All the inspectory findings are confirmed.
Fluid thrill is absent .
Shifting dullness present .
Liver is not palpable
Spleen is not palpable.
Percussion :
Tympanic note in the anterior aspect of abdomen
Dull note in the flanks of abdomen.
Liver dullness is present .
Auscultation :
Bowel sounds present .
Diagnosis :
ASCITIS UNDER EVALUATION.
INVESTIGATIONS :
Ascitic fluid analysis:
Ascitic fluid tapping was done on 13/2/23.
Diagnostic Ascitic fluid tapping on 16/2/23
ECG :
2D ECHO :
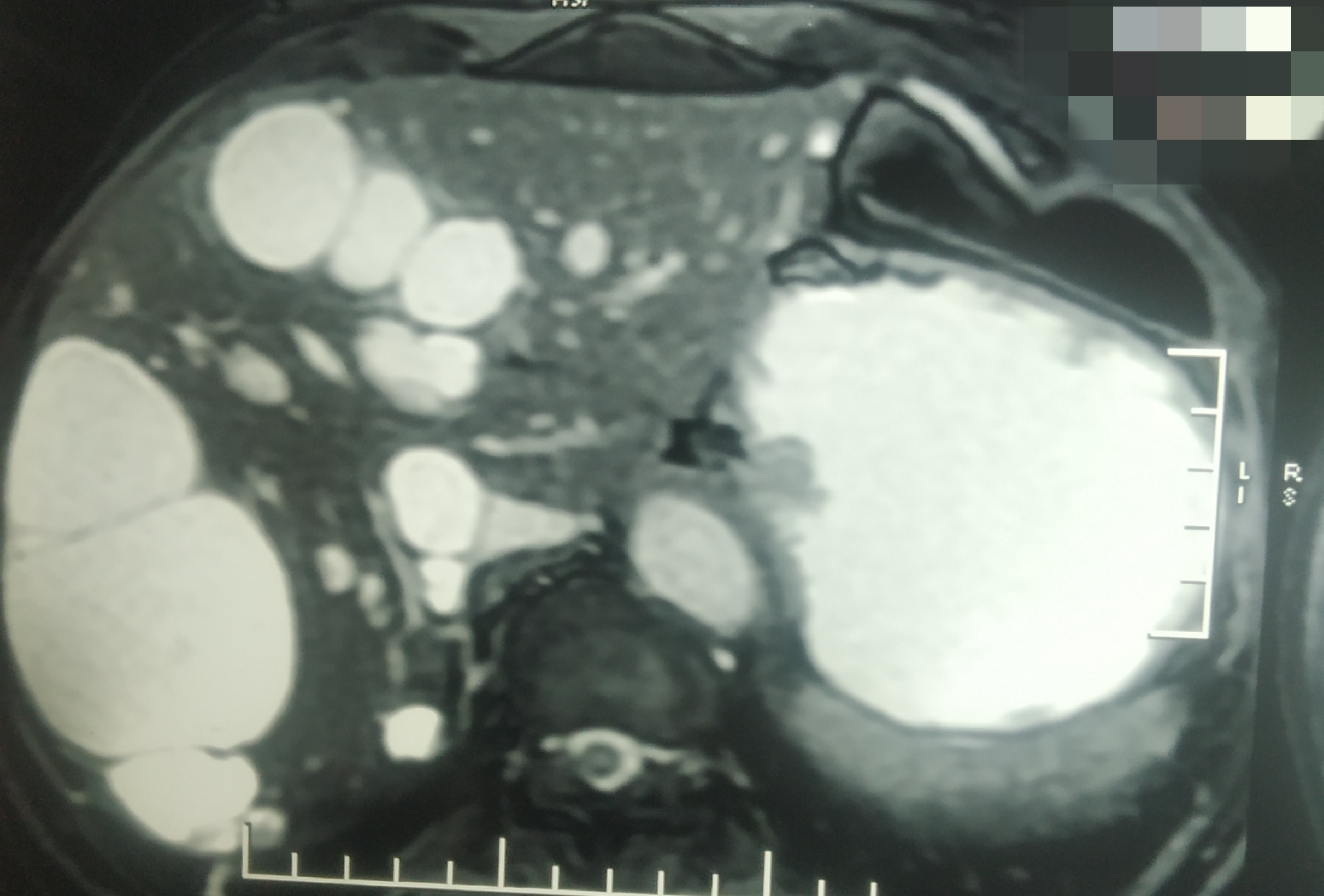
1. E/O multiple cysts in both lobes of liver with septations largest measuring 94mmx30mm
2. E/O 44mmx 60mm anechoic cyst noted in the mid pole of left kidney
3. Epigastric hernia with omentum as herniating content .
4. Moderate ascitis .
DIAGNOSIS :
Moderate Ascitis
Low saag high protein (Cells 560 )
? Spontaneous bacterial peritonitis
Multiple cysts in hepatic and renal ( single )
?PCKD
With epigastric hernia
TREATMENT :
1. Fluid restriction <1litre per day
2. Salt restriction <1.2gm per day
3. Inj. Lasix 40mg IV/BD
4. Inj. Monocef 1gm IV /BD
5. Inj. PCM 1GM IV/SOS ( if temperature more than 101F)
6. Inj. Tramadol IV/SOS
7. Tab. Rantac 150mg PO/OD.
































Comments
Post a Comment